Your Asthma Management Plan is essential written guides that help you manage your asthma effectively.
There are 3 core elements to your Asthma Management Plan:
- A plan of the routine medication that your patient should take to stay well
- What to do if asthma symptoms worsen
- What to do in the case of an asthma attack and when to call 999.
These three stages are traffic lighted green (routine), yellow (warning that control is starting to slip ) and red (emergency).
To download your Asthma Management Plan click here:
How to use your Asthma Management Plan
Your Asthma Management Plan can help you stay on top of your asthma. To get the most from it you could:
- Download and print the document and put it somewhere easy to find – your fridge door, noticeboard or bedside table.
- Keep a photo of it on your mobile phone or tablet – so you can check it wherever you are. You can also send it to a family member or friend, so they know what to do if your asthma symptoms get worse.
- Check in with it regularly – put a note on your calendar or a monthly reminder on your phone to read it through. Are you remembering to use your everyday asthma medicines? Do you know what to do if your symptoms get worse?

Do you require further advice and support?
- You can contact Asthma + Lung UK for further advice and support regarding your Asthma in the following ways:
- Speak to a respiratory nurse specialist about managing your asthma: 0300 222 5800 (Monday to Friday, 9am to 5pm)
- Message an Asthma + Lung UK specialist asthma nurses on Whatsapp: 07378 606728 (Monday to Friday, 9am to 5pm)
- Get news, advice and download information: AsthmaAndLung.org.uk
- Follow Asthma + Lung UK on Facebook for news and tips about your asthma: Facebook.com/AsthmaLungUK
- You can contact the practice in the following ways and ask to book an appointment with the practice nurse (face to face or over the telephone):
- Telephone: 0151 902 0020
- Email: Cornerways.mc@nhs.net
How often will I be reviewed?
You will be invited for an asthma review at least once per year.
Prior to your appointment you will be asked to complete a brief questionnaire related to your asthma, e.g. how well you feel. The questionnaire will be sent to you via SMS and when you complete it all answers will be updated into your medical record. If you are unable to complete the questionnaire or do not have a mobile phone then one of our team will call you to complete the questionnaire over the telephone.
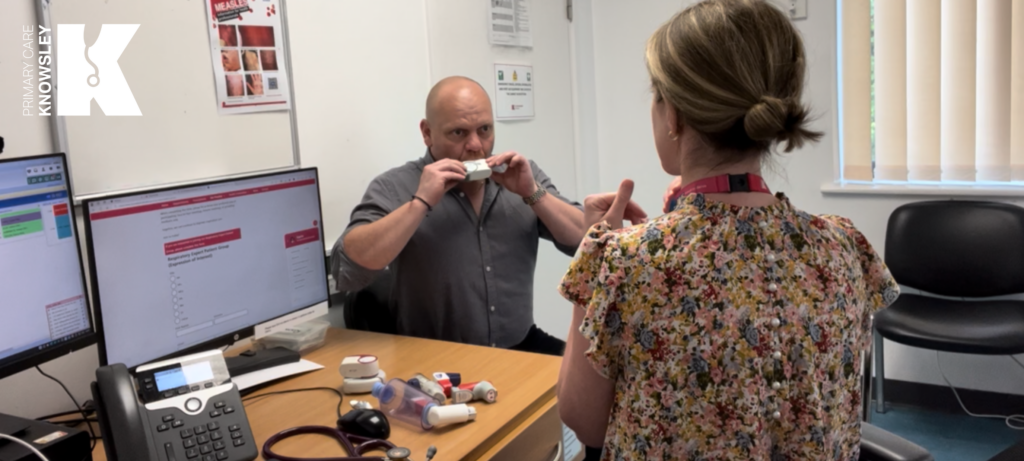
When attending an appointment with the Practice Nurse you should always bring with you:
- any inhalers and spacers you have, to check you are using them correctly and in the best way ·
- your peak flow meter if you use one
- any questions you have about your asthma and how best to manage and cope with it.


Your Everyday Asthma Care
You will be provided with a plan to manage your asthma on a daily basis, It is important you stick to this routine to ensure that you keep well and your asthma is being managed regardless of how you are feeling!
Preventer Inhaler
You will be given a plan for the number of puffs you should take from your preventer inhaler in the morning and at night on a daily basis. You will need to ensure you keep to this routine.
Reliever Inhaler
You should only take your reliever inhaler when you need to which may include you when:
- you are wheezing
- your chest feels tight
- you find it hard to breath
- you are coughing
Other medicines/devices
You may also be provided other medicines and devices to help support the management of your asthma, e.g. spacer or a peak flow metre. Please ensure you use what has been ‘prescribed’ and keep to the routine and advice.

When you are managing your asthma well you should expect/aim:
- to have no symptoms
- to not require your reliever inhaler for at least 12 weeks

When you feel worse
When your asthma is getting worse you may experience any of the following:
- Your symptoms are coming back, e.g. you may experience wheezing, tightness in your chest, you may feel breathless or cough
- You may be waking up at night
- Your symptoms may be interfering with your usual day-to-day activities (e.g., work, exercising)
- You may be using your reliever inhaler three times a week or more.
URGENT!
If you need your reliever inhaler more than every four hours, you need to take emergency action now. See section ‘When I have an Asthma Attack’
If you haven’t been using your preventer inhaler, you should start using it regularly again or if you have been using it:
- You will be provided with a plan to increase the number of puffs from your preventer inhaler until your symptoms have gone and your peak flow is back to your personal best
- Take your reliever inhaler as needed, ensuring you do not go over the maximum number of puffs as directed by your Practice Nurse
- Carry your reliever inhaler with you when you’re out and about.
Header text
URGENT!
You should see a doctor or nurse within 24 hours if you get worse at any time or you haven’t improved after seven days.


When you have an Asthma Attack
You will be having an asthma attack if you are experiencing any of these:
- Your reliever inhaler is not helping or you need it more than every four hours.
- You find it difficult to walk or talk.
- You find it difficult to breathe
- You are wheezing a lot, or you have a very tight chest, or you are coughing a lot.
- When your peak flow is below the number as directed by your Practice Nurse.

What to do in an Asthma Attack
- Sit up straight – try to keep calm.
- Take one puff of your reliever inhaler (usually blue) every 30-60 seconds up to 10 puffs.
- If you feel worse at any point OR you don’t feel better after 10 puffs call 999 for an ambulance.
- If the ambulance has not arrived after 10 minutes and your symptoms are not improving, repeat step 2.
- If your symptoms are no better after repeating step 2, and the ambulance has still not arrived, contact 999 again immediately.
Important:
This asthma attack advice does not apply to you if you use a MART inhaler.

What to do after an Asthma Attack
- If you dealt with your asthma attack at home, see your GP today.
- If you were treated in hospital, see your GP within 48 hours of being discharged.
- Finish any medicines they prescribe you, even if you start to feel better.
- If you don’t improve after treatment, see your GP urgently
Educational Resources
What is Asthma (Video)
How to get your breath back! (Video)
How to manage an asthma attack (Video)
How to use my inhaler (Link to Video)
Click Here for more educational videos on different inhalers (Asthma + Lung UK)
